Provider Pulse – July 2022
 Sign Up for EFT to Get Claims Paid Faster
Sign Up for EFT to Get Claims Paid Faster
Electronic funds transfer (EFT) gets your claims paid fast and more accurately. Sign up for EFT today! It’s as easy as these simple steps:
- Visit www.TriWest.com/ClaimsInformation.
- Find the "PGBA EFT/ERA Enrollment Package."
- Complete the forms and submit them to PGBA.
If you haven’t yet reestablished EFT through TriWest’s new claims processor, PGBA, please encourage your billing team to take the time to set it up today!
 VA Expands Live Donor Transplant Care and Support within VA CCN Contracts
VA Expands Live Donor Transplant Care and Support within VA CCN Contracts
The Department of Veterans Affairs (VA) Community Care Network (CCN) contracts now provide support for procedures and related care to those who donate an organ or bone marrow for transplantation into Veterans, effective as of July 1, 2022.
This expanded benefit within the VA Community Care Network (CCN) contracts provides care and coverage for live donors throughout the donation process, to include:
- Initial screening and eligibility determination for anyone interested in donating a solid organ or bone marrow to a Veteran
- Pre-donation testing and evaluation
- Solid organ or bone marrow donation procedure
- Post-donation care for up to a two-year period
- Associated travel and lodging expenses
Live donors donating their organ or bone marrow to a Veteran transplant recipient may receive care and services associated with the donation within VA or in the community. VA Community Care Network (CCN) contracts for Regions 1-4 have been modified to include live donor coverage through in-network community providers for transplant services.
If determined by the transplant provider that live donation is an option for the Veteran transplant recipient, VA Medical Center (VAMC) may authorize live donor’s care at a CCN in-network transplant facility. Separate VA authorization is required for live donor follow-up care after organ or bone marrow donation. The referring VAMC Referral Coordinator will be responsible for full coordination of the live donor community referral and care process and will remain as the primary the point of contact for any questions related to transplantation or organ donation.
For more details on the live donor transplant process, please refer to the Live Donor Transplant Care and Support reference guide.
 IMPORTANT: SEOC Changes for Veteran Home Health Care
IMPORTANT: SEOC Changes for Veteran Home Health Care
The Department of Veterans Affairs (VA) has updated and implemented new Standardized Episodes of Care (SEOC) pertaining to the authorization of adult day health care, homemaker/home health aide, in home respite, and skilled home health care services, effective June 23, 2022. These changes allow the VA’s Geriatric Extended Care (GEC) Program Office greater flexibility, and enhance the coordination of these services.
Please note the following new SEOCs and time durations:
Community Adult Day Health Care Services
- 1 Day Per Week, 30, 90, 180 and 365 Days
- 2 Days Per Week, 30, 90, 180 and 365 Days
- 3 Days Per Week, 30, 90, 180 and 365 Days
- 4 Days Per Week, 30, 90, 180 and 365 Days
- 5 to 7 Days Per Week, 30, 90, 180 and 365 Days
Homemaker/Home Health Aide
- 106 to 168 hours Per Week, 30, 90, 180 and 365 Days
- 21 to 36 hours Per Week, 30, 90, 180 and 365 Days
- 37 to 58 hours Per Week, 30, 90, 180 and 365 Days
- 59 to 105 hours Per Week, 30, 90, 180 and 365 Days
- Up to 20 hours Per Week, 30, 90, 180 and 365 Days
In Home Respite
- 106 to 168 hours Per Week, 30, 90, 180 and 365 Days
- 21 to 36 hours Per Week, 30, 90, 180 and 365 Days
- 37 to 58 hours Per Week, 30, 90, 180 and 365 Days
- 59 to 105 hours Per Week, 30, 90, 180 and 365 Days
- Up to 20 hours Per Week, 30, 90, 180 and 365 Days
Skilled Home Health Care Bundled, Non-Bundled, Expanded
- Bundled: 30, 60, 120 and 180 Days
- Non Bundled: 30, 60, 120 and 180 Days
- Expanded: 30, 60, 120 and 180 Days
Discontinued SEOCs:
- Community Adult Day Health Care Case Mix ABC
- Community Adult Day Health Care Case Mix DEFGHI
- Community Adult Day Health Care Case Mix JK
- Community Adult Day Health Care Case Mix L
- Community Adult Day Health Care Case Mix Exception
- Homemaker-Home Health Aide Case Mix A, B, or C
- Homemaker-Home Health Aide Case Mix D, E, or F
- Homemaker-Home Health Aide Case Mix G, H, or I
- Homemaker-Home Health Aide Case Mix J, or K
- Homemaker-Home Health Aide Case Mix L
- Homemaker-Home Health Aide Exception
- In Home Respite Case Mix A, B, or C
- In Home Respite Case Mix D, E, or F
- In Home Respite Case Mix G, H, or I
- In Home Respite Case Mix J or K
- In Home Respite Case Mix L
- In Home Respite Case Mix Exception
- Skilled Home Health Care Bundled
- Skilled Home Health Care Expanded
- Skilled Home Health Care Non Bundled
Existing authorizations for care will be honored for the dates indicated on the authorization. The VA may evaluate current authorizations and submit new referrals with amended dates of service to better facilitate coordination of Veteran care.
For additional information regarding authorized care, please refer to the authorization letter, Referral and authorization process QRG, and VA’s SEOC code list.
 Sign Up for New Claims Provider Reporting Tool
Sign Up for New Claims Provider Reporting Tool
The Provider Reporting Tool is a new resource for providers to receive one-time, weekly or monthly claims status reports sent via email. It is helping eliminate the need for a provider to call in for answers to simple status inquiries. Reports can be sent to up to five email addresses at a time.
TriWest recently launched the tool and has already received some positive feedback from providers who are now receiving reports right to their inbox, including:
- “The reporting tool provides us the information our team needs and does not require us to make a call unless we are disputing a denial or have a question.”
- “Since we are getting the report, we rely less on calling into your call center. The billing team prefers working from the report.”
To subscribe and begin receiving claims status reports, contact the TriWest Claims Call Center at 877-226-8749. The report is currently ONLY available by contacting TriWest.
 REMINDER - VA Required Medical Records for all CCN Services
REMINDER - VA Required Medical Records for all CCN Services
As a part of the VA Community Care Network, medical records and documentation are required for all provided services. Providers are required to submit medical documentation directly to the authorizing the VA Medical Center (VAMC), preferably via upload to VA’s HealthShare Referral Manager (HSRM).
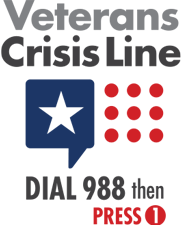
Providers should submit urgent and emergent care documentation as soon as it is complete. Standard, urgent and high-priority timeframes may apply based on the type of care provided. Referrals to screen for cancer or to treat a suicidal Veteran are other examples of high priority medical documentation to return quickly.
Detailed and complete reports relating to care are important for quality assurance of Veteran care. For example, a pathology report should be included when sending medical documentation after a colonoscopy.
All medical documentation must be signed (written or electronic), and/or initiated by the submitting provider or practitioner. In addition, no release of information (ROI) is required.
VA requires providers submit medical documentation to the authorizing VAMC or Veteran’s assigned VAMC within the following timeframes:
- Initial medical documentation for outpatient care – within 30 days of the initial appointment
- Final outpatient medical documentation – within 30 days after the completion of the Standardized Episode of Care (SEOC)
- Medical documentation for inpatient care – within 30 days, and will consist of a discharge summary
- Any medical documentation requested by VA for urgent follow up – upon request
For more information, refer to the Medical Records and Documentation Requirements Quick Reference Guide.
 Provider Handbook Updates
Provider Handbook Updates
The CCN Provider Handbook will soon include the expanded live donor transplant information as described above.