Provider Pulse – May 2023
 Subscribe to VA's Provider Advisor
Subscribe to VA's Provider Advisor
Get access to the more Veteran health news when you subscribe to the Provider Advisor, the monthly newsletter from the Department of Veterans Affairs (VA).
For timely, informative and useful VA health news, subscribe to Provider Advisor. Enter your email and create a password for "Email Updates" and then select from a variety of VA news you'd like to receive.
 Time Codes for Massage Therapy SEOCs Limited
Time Codes for Massage Therapy SEOCs Limited
Under the direction of VA and to better align with Standard Episode of Care (SEOC) language, TriWest Healthcare Alliance (TriWest) limits massage therapy timed codes to 60 minutes for the initial visit and massage therapy treatment.
Additionally, follow-up sessions are limited to 30 minutes unless it is a complex condition as defined in the procedural overview on the Massage Therapy SEOC letter.
This is not a change, but a reminder to adhere to the limitations outlined in the SEOC referral letter.
This guidance is specific to the PMR_MASSAGE THERAPY (MEDICAL) - ACUTE PAIN and PMR_MASSAGE THERAPY (MEDICAL) - CHRONIC PAIN SEOCs, and does not apply to other SEOCs such as chiropractic or physical therapy SEOCs.
Apply "Always Therapy" Codes
According to the Centers for Medicare & Medicaid Services (CMS), outpatient services furnished by therapists in private practices (TPPs) are always considered therapy services regardless of whether they are designated as "always therapy" or "sometimes therapy." The appropriate therapy modifier must be included on the claim.
If a claim has an "always therapy" code, it must be appended with one of the therapy modifiers to indicate the plan of care under which the massage therapy was furnished:
- GN: Speech-language pathology
- GO: Occupational therapy
- GP: Physical therapy
If one of these modifiers is not included, the claim will be denied.
It may be clinically appropriate for physicians and TPPs to furnish outpatient services that have been designated "sometimes therapy" codes outside a therapy plan of care. In these cases, therapy modifiers are not required and claims may be processed without them.
For more information on how to apply these codes please refer to the Massage Therapy Billing Quick Reference Guide. This QRG can also be found on TriWest's Payer Space at Availity.com.
 Reminder: Do Not Solicit for Veteran Referrals
Reminder: Do Not Solicit for Veteran Referrals
As a reminder, network providers are not permitted to solicit VA or Veterans for referrals.
All care must be referred by VA unless it's for urgent/emergent services.
A provision under provider contracts with TriWest specifically states: "Provider shall not advertise the award of the Agreement or these T&C in its commercial advertising in such a manner as to state or imply that the Department of Veterans Affairs endorses a product, project or commercial line of endeavor."
Examples of soliciting can include distributing flyers, publishing advertisements about services to Veterans, etc.
If you are interested in sharing with your community that you serve Veterans, providers can promote their services using our Proudly Caring materials found on the Proudly Caring for Veterans web page on the TriWest website. You can download either a PDF print-ready sign or a website badge for online presence.
 CAH Providers to Bill Claims with GT Modifier for Telehealth Services
CAH Providers to Bill Claims with GT Modifier for Telehealth Services
Critical Access Hospital (CAH) providers are required to bill claims on a UB-04/Institutional claim and append the modifier GT when billing any Telehealth service provided to a Veteran via interactive audio and/or video telecommunications systems.
As a reminder, the GT modifier should not be added to any other Telehealth services when performed by other provider types.
Any claims submitted by other provider types that include the GT modifier will be rejected and returned to submitter.
For more information visit the Telehealth Guidelines web page.
 Emergency Suicide Care Treatment for Veterans: COMPACT Act Update
Emergency Suicide Care Treatment for Veterans: COMPACT Act Update
As a result of the Veterans COMPACT Act of 2020, emergent suicide care for eligible Veterans in acute suicidal crisis at a VA or non-VA facility is a covered benefit. VA has updated COMPACT Act guidelines for acute suicidal crisis care for Veterans.
Veterans meeting certain criteria are eligible for urgent care or emergent care if in an acute suicidal crisis. A trained crisis responder or health care provider must also diagnose the Veteran's eligibility using given criteria, in order to enable this benefit.
Read more about the COMPACT Act and Veteran coverage for acute suicidal crisis in the CCN Urgent Care & Emergent Care Quick Reference Guide.
 Review the National Drug Code Billing Guidelines
Review the National Drug Code Billing Guidelines
As a reminder, when billing claims with drug codes on a CMS 1500 form (professional), electronic 837P, UB-04 (institution) and/or electronic 837I, it is necessary to bill the NDC number, units and quantity correctly.
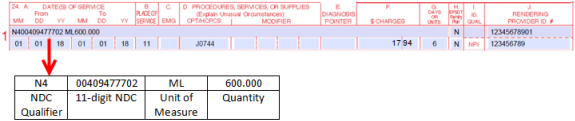
Professional Paper Claim Guidelines (CMS-1500)
In the shaded portion of the line-item field 24A-24G on the CMS-1500, enter the qualifier N4 (left-justified), immediately followed by the NDC. Next, enter one space for separation, then enter the appropriate qualifier for the correct dispensing unit of measure (UN, ML, GR, or F2), followed by the quantity (number of NDC units up to three decimal places), as indicated in the example below.
Institutional Paper Claim Guidelines (UB-04)
In the line-item field 42-46, enter the appropriate drug-related revenue code in field 42. In field 43, report the NDC qualifier N4 (left-justified), immediately followed by the 11-character NDC in the 5-4-2 format (no hyphens). Immediately after the last digit of the NDC, enter the appropriate qualifier for the correct package size, NDC unit of measure (UN, ML, GR, or F2), followed by the quantity (number of NDC units up to three decimal places), as indicated in the example below.
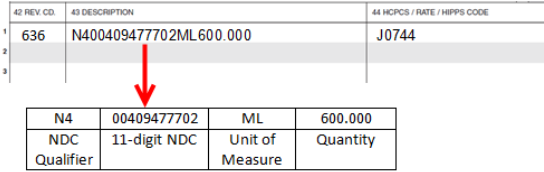
Be sure to include the N4 before the 11-digit NDC number, but do not include drug name on the claim form. If the drug name is included on the claim form, this may result in the claim being denied.
For more information see the Professional Claims Basics Quick Reference Guide.





