Provider Pulse – June 2022
 Get Claims Paid Faster with EFT
Get Claims Paid Faster with EFT
With electronic funds transfer (EFT), you can get your claims paid faster and more accurately. Paper checks are subject to error if the wrong information has been entered, and receipt of your check depends on the pace of the post office — your payment can be mailed to the wrong office, get pushed to a different shipment, and take much longer to fulfill if anything goes wrong.
To avoid delays and settle your accounts quickly, sign up for EFT today! It’s as easy as these simple steps:
- Visit www.TriWest.com/ClaimsInformation.
- Find the "PGBA EFT/ERA Enrollment Package."
- Complete and submit the forms to PGBA.
If you haven’t yet reestablished EFT through TriWest’s new claims processor, PGBA, please encourage your billing team to set it up today.
 Rx Buy and Bill: Understand the Process
Rx Buy and Bill: Understand the Process
Buy and Bill is an existing procedure for providers to obtain specialty medications that require administration to patients in the office. The "buy" refers to the order and purchase of the medication to dispense in the office. The "bill" refers to providers billing directly to TriWest for reimbursement.
Providers who administer drugs to Veteran patients in their offices are required by TriWest to follow CCN’s Buy and Bill process. While most of these types of medications are available from a specialty pharmacy, not all are currently available as a pharmacy benefit. Therefore, providers must obtain their prescription drugs from a specialty distributor - not a specialty pharmacy.
Providers can purchase the medication from a specialty distributor (specialty pharmacies are one type of distributor but this includes all specialty distributors). Depending on the medication or product, the provider may order one or buy in bulk to keep on hand in their office.
Follow the Buy and Bill Process
Providers who want to participate in CCN’s Buy and Bill process should follow the process outlined below for specialty medications:
- Ensure the medication is covered for the condition referred under the issued Standard Episode of Care (SEOC). The treatment using the specialty medication should have a valid J code entered on the claim and must be FDA-approved. Investigate benefits (prior authorizations may be required) at Department of Veterans Affairs (VA) Formulary Advisor.
- Write a prescription for the medication.
- Order and receive medication from specialty distributor. Store and monitor inventory appropriately.
- Administer the medication to the Veteran and document in medical record.
- Submit medical claim for procurement and administration to TriWest (not a pharmacy claim through a PBM).
- Receive reimbursement from TriWest.
For more details about the Buy and Bill process, including using the proper codes and provider responsibilities, refer to the Buy and Bill Quick Reference Guide.
 Clean Claims Reminder for Ancillary Providers
Clean Claims Reminder for Ancillary Providers
For a claim to process and pay properly, TriWest needs to have visibility to the appointment in our systems. Once a provider receives an authorization letter from either TriWest or the Department of Veterans Affairs (VA), this referral/authorization number is the unique identifier assigned for each approved referral/authorization’s episode of care.
To help improve claims payment accuracy, the VA referral/authorization number is required with all VA Community Care Network (CCN) claims submissions.
Providers are required to share the VA referral/authorization number with ancillary providers who are included in a Veteran’s episode of care. The ancillary provider is also required to use this same VA referral/authorization number when submitting their claim for the specific episode of care.
If this referral/authorization number is not used on the claim, the claim will be denied. The only exception is urgent care.
Use the Correct Format
The 10-digit VA referral number must be included. Avoid extra spaces, characters or words. A "clean" VA referral number looks like this: VA0012345679.
Insert the VA referral number in the following claims forms in specific locations:
- CMS 1500: Box 23 Prior Authorization Number field
- CMS UB04: Box 63 Treatment Authorization Codes field
- EDI – two options:
- 2300 – REF (G1) Prior Authorization
- 2300 – REF (9F) Referral Number
For more information regarding clean claims, please refer to the Provider Handbook or the Claims Basics Quick Reference Guide.
 VA and TriWest Training Offers Continued Education, Policy Updates
VA and TriWest Training Offers Continued Education, Policy Updates
Interested in continued learning to help you better serve Veterans? Both VA and TriWest offer training opportunities on various topics to support the important work you do.
VA Training Opportunities
VHA Office of Integrated Care Programs and Policies Overview – A live webinar that includes background on community care and corresponding VA regulations. In-depth discussions will be held on topics such as referrals and authorizations, authorized and unauthorized emergency care, urgent care, claims, and more.
- The next live webinar will take place on July 21 at 10 a.m. MST.
- A similar webinar is planned for August 2022.
Pain Management and Opioid Safety in VHA – This recorded, knowledge-based webinar will provide updated information to community care providers and health care teams about VHA Pain Management approaches and the VA Opioid Safety Initiative.
- MISSION Act Section 131: Opioid Safety Initiative
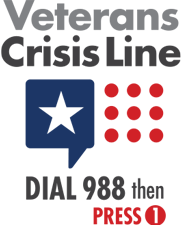
Preventing Suicide Through Safety Planning and Lethal Means Safety – This recorded, virtual training will provide health care teams with key data and research updates on the national problem of Veteran suicide.
- MISSION Act Section 133: Preventing Suicide Through Lethal Means and Safety Planning
War Related Illness and Injury Study Center (WRIISC) – A national program in VA’s Post-Deployment Health Services provides expertise to Veterans and providers on difficult to diagnose illnesses and environmental exposure concerns.
- Module 1 (Assessing Deployment Related Exposures) – The first in a series of post-deployment health, web-based training modules. It provides clinically relevant knowledge on the role of environmental exposures in Veteran health, and the importance of addressing each patient’s exposure concerns. Course participants will learn how to conduct a deployment-related exposure assessment and determine whether an exposure could be associated with a Veteran’s specific health concern.
- To register for this class or to access available sessions, log in to VA’s training website VHA TRAIN. Check the VHA TRAIN website for more information and other upcoming sessions.
TriWest Training Opportunities
Upcoming Change in Policy to Live Donor Transplant Care for Veterans – There is an expected change in policy coming from the Department of Veterans Affairs (VA) regarding live donor transplant care for Veterans.
TriWest will host webinar trainings to help explain the details of this upcoming policy change.
Please plan to attend one of the following webinar training dates:
- July 7, 2022 at 4 p.m. EST
- July 19, 2022 at 1 p.m. EST
Register Now!
To register for the training, follow the steps below:
- Log into Availity at: www.availity.com.
- Navigate to "TriWest Payer Space" (under the "Payer Spaces" tab).
- Click on "Access TriWest Learning Center" on the main page.
- Click "Sessions" from the top navigation.
- Find the course, click "View Course" then "Enroll" at the top right of the page.
After you register, a link to the webinar training and login credentials will be emailed to you.
The webinar is hosted via Zoom and will include live question-and-answer sessions, and a link to download the presentation slides.
 Provider Handbook Updates
Provider Handbook Updates
The following language has been added to page 18 of the CCN Provider Handbook:
VA Requires Signature on File for CCN Claims
As a requirement of participation in the Department of Veterans Affairs (VA) Community Care Network (CCN), network providers need to have a Signature on File for any Veteran who will receive care. Similar to standard insurance policies, the Signature on File will indicate that the provider is authorized to submit a claim on behalf of the Veteran, and authorizes payment of medical benefits to the provider.