
Provider Pulse
November 2017
Welcome to November
The month of Thanksgiving has finally arrived! And we have lots of things happening at TriWest. Read below for our tips on navigating the new authorization letters, as well as a heads up on why you might receive a call from TriWest. Happy Thanksgiving!
In This Edition:
How to Navigate the New Authorization Letters
In case you haven’t noticed, the TriWest authorization letters have changed in format. These changes made them simpler, shorter and easier to navigate.
The changes officially launched on Sept. 29, 2017. The biggest change involves secondary authorization requests, or SARs.
- If you need to refer to a different provider with a different TIN, as long as your authorization includes the care, you do NOT need to send a SAR anymore.
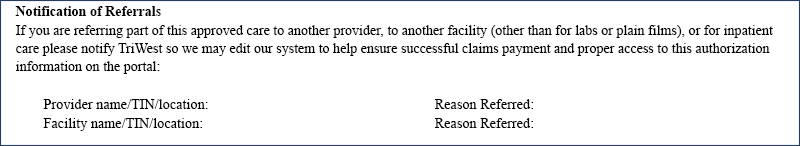
- Instead, fill out the “Notification of Referrals” section on the second page of your authorization letter. Then, fax it back to TriWest at 1-866-259-0311.
- However, if your authorization doesn’t include the necessary care and you have to refer to a different provider with a different TIN, still submit a SAR to TriWest.
The Two Types of Authorization Letters
To align with changing industry standards, TriWest and the Department of Veterans Affairs (VA) are evolving to a more standardized, Medicare-centric model. Therefore, TriWest has two types of authorization letters:
- Standardized Episodes of Care, or SEOCs: this affects nine specialties. You will know if you have an SEOC authorization because the letter will say it on the first page.
- Non-SEOC letters: all other authorization letters.
Eventually, TriWest and VA hope to evolve all authorizations to an SEOC model.
What’s Covered?
To understand what’s covered for SEOCs, please refer to the “narrative language” on the first page of the letter.
For all other authorization letters (non-SEOCs), the letters list the CPT codes of the approved services. For these situations, you may still use the list of authorized codes on the TriWest Provider Portal available at www.triwest.com/provider/authorization-codes.
For more information on the new authorization letters, please review our Authorization Letter Quick Reference Guide.
NEWS BULLETIN: Changes in Health Care Models Affecting VA
Changes to health care models are not coming. They are here.
VA is taking notice and evolving its authorization model to align with the changing industry.
The alphabet soup of new programs and initiatives is a clear indicator that some federal programs are transitioning from fee-for-service to value-based models; MACRA, QPP, APM and MIPS are just a few examples. The goal of these health care models is better management of resources and the reduction of costs without lowering quality of care.
The SEOC Model
To address growing health care demands in a fiscally and clinically responsible manner, VA is implementing a new model for how services are authorized – the Standardized Episode of Care – or SEOC model. An SEOC allows VA to bundle the types and quantities of services, while still following Medicare’s fee-for-service approach. VA’s innovative SEOCs help reduce overuse, manage costs and ensure Veterans nationwide have access to appropriate services while minimizing administrative burdens on provider offices.
Benefits for Providers
When a physician is familiar with a diagnosis or procedure, standing orders are often utilized. Standing orders provide optimal care for the majority of patients. SEOCs offer similar benefits.
VA recognizes that most episodes of care have a reasonably predictable number, duration and type of services during a course of treatment. Pre-approved SEOC templates establish a national standard, lower the administrative burden, reduce delays in care and help control costs. When necessary care falls outside the predictable range, providers can request additional authorization. Clinical documentation helps support this approach and allows each VA Medical Center to manage care in conjunction with community providers.
Unlike other bundled models, TriWest pays providers on the individual codes billed. Therefore, payment may vary from Veteran to Veteran.
Faster, simpler and standardized, SEOCs are a clinically responsive solution allowing VA to manage care and costs responsibly!
TriWest Might Call You
You saw a Veteran patient with a TriWest authorization. You meant to file your claim and submit your medical documentation, but time got away from you.
The next thing you know, 21 days have passed and you get a call from TriWest.
"Hello," the TriWest representative says. "We're calling to see if the Veteran showed up to his or her appointment? We never received your medical documentation or a claim."
Why the Call?
Starting Oct. 30, 2017, TriWest began calling providers 21 days after Veteran appointments if providers have not submitted medical documentation and a claim yet. The rollout started with certain specialties and will eventually become network-wide.
We’re starting this policy to confirm Veterans actually go to their appointments. If you–the provider–do not file claims or submit medical documentation within 21 days, it raises a flag that the Veteran may have been a no-show. Most helpful is when you notify us proactively that a Veteran is a no-show, in which case we would not initiate the 21-day call. We very much appreciate that collaboration.
TriWest is working in partnership with VA to ensure coordination of care for Veterans. This is merely one more step in that process.
Additionally, VA requires providers submit medical documentation within certain timeframes, and TriWest encourages providers to submit claims within 30 days of rendering services. This phone call may also act as a friendly reminder for both these tasks.













