
Provider Pulse
March 2018
Welcome to March – SEOC Month
March is here, and we have a special edition for you! Over the past few months, TriWest began transitioning many of its authorization letters to a new format called "Standardized Episodes of Care," or SEOCs. These SEOCs are a new, more comprehensive model of ordering health care driven by the Department of Veterans Affairs (VA) to improve consistency across all VA Medical Centers. They were developed to decrease your administrative burden and improve continuity of care for Veterans.
We know the transition has caused some questions, so we dedicated this month's Provider Pulse to SEOCs. Plus, we launched a new SEOC webinar to help you understand how SEOCs work. Register now!
In This Edition:
What are SEOCs?
Standardized Episodes of Care (SEOC) are a new, more comprehensive model of ordering health care driven by the Department of Veterans Affairs (VA) to improve consistency across all VA Medical Centers (VAMC).
They were developed to decrease your administrative burden and improve continuity of care for Veterans. With SEOCs, you won’t need to submit as many secondary authorization requests (SAR) and will have more freedom to provide clinically appropriate services.
[Not sure if you need a SAR? Visit the TriWest SAR Decision tool at www.triwest.com/provider-SAR.]
Each Specialty Has Its Own SEOC
Each specialty has its own SEOC template authorizing a standardized, minimum amount of care that must be allowed when medically necessary. VAMCs may add to the template’s minimum, but may never take away from it. Some SEOCs may authorize more care than your office needs to provide. In such cases, only provide and bill what is clinically necessary.
TriWest has been converting its authorizations to SEOC formats by specialty type; however, not all authorizations have been converted yet. The rollout is happening rapidly in phases. To determine whether you have an SEOC, review our SEOC Quick Reference Guide.
For more information on SEOCs, you may also register for our new live, interactive webinar!
How to Read a SEOC
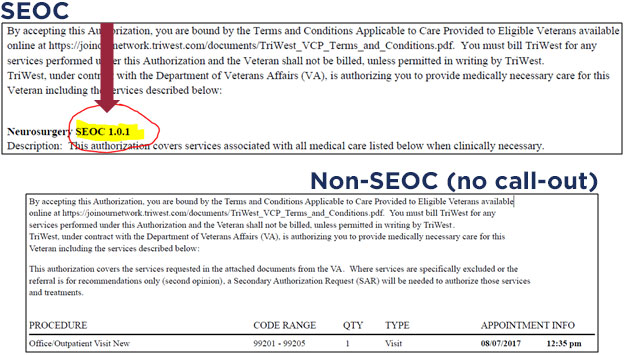
Not all authorizations have converted to an SEOC format yet. Below is an example of an SEOC authorization versus a non-SEOC authorization. As you can see, the SEOC has a call-out that labels it as such.
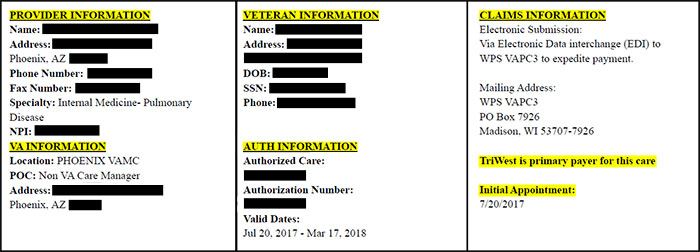
The "Face Sheet"
At the top of your SEOC will be a Face Sheet. This gives basic information, such as the Veteran name and address, the contact information for the overseeing VAMC, and the authorization number.
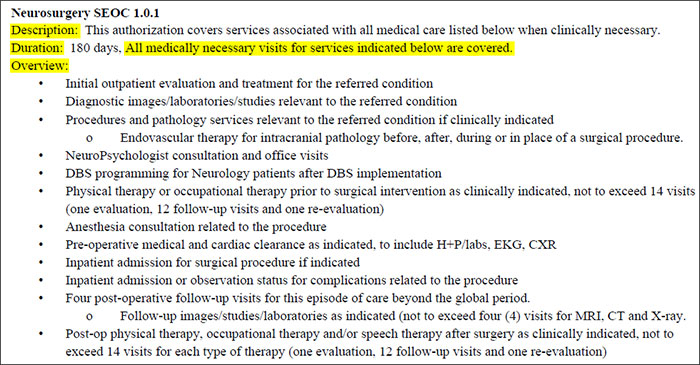
The "Narrative"
The Narrative of the SEOC describes HOW you may administer the services that have been approved. It will frequently include information such as whether you’re pre-authorized to refer to another type of provider, or if you may send the Veteran for follow-up care. The Narrative will also clarify how many office visits have been authorized under the “Duration” section. Read the Narrative carefully!
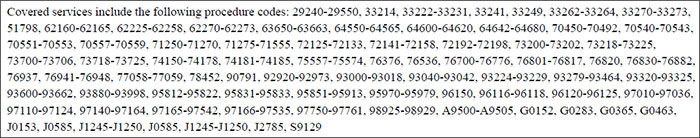
The "Code Range"
This section of the SEOC clarifies WHAT services are covered. The Code Range lists the ranges of all CPT codes authorized. When determining what’s covered under a SEOC, you need to read both the Narrative AND the Code Range; they work together.
Need More Help Understanding SEOCs?
We have a fantastic live, interactive webinar on SEOCs just for you. Register for the SEOC Webinar now! It’s completely free.
4 Times You Need a SAR for SEOCs
Did you know that half of all secondary authorization requests–or SARs–that TriWest receives are unnecessary? With SEOCs, the need to submit SARs goes down even more. So how do you know when it’s appropriate to send a SAR?
The SAR Decision Tool
TriWest has developed a SAR Decision Tool to help you determine if you truly need one. Before you submit a SAR, be sure to visit the SAR Decision Tool first, at www.triwest.com/provider-SAR.
4 Times You Need a SAR
When reviewing your SEOC, pay close attention to both the Narrative AND Code Range sections, as well as any clinical consult materials provided. After reviewing all areas thoroughly, if you believe the services you need are still not covered, you may need a SAR.
The four times a SAR may be necessary for a SEOC:
- You’re referring to another provider who has a different TIN.
- You’re requesting care for a condition other than what was referred in the SEOC.
- You’re extending the valid date range on your SEOC or adding additional visits beyond what was authorized.
- You’re adding a CPT code (additional services) not included on your SEOC Code Range.
How to Submit a SAR
If you think you may need a SAR, follow these steps to submit one:
- Access the SAR Decision Tool at www.triwest.com/provider-SAR to confirm whether a SAR is necessary. If so, the tool will provide a link to the SAR 15 form.
- The request for care should include:
- Completed SAR 15 Form
- Notes
- Discharge plans (if applicable)
- Medical documentation justifying the request for additional services
- Submit the completed SAR to TriWest by fax to: 1-866-259-0311.
Other SEOC Resources
We understand that SEOCs are a new model of receiving authorizations. You may have multiple questions, even after reading our Provider Pulse edition this month.
Below are other resources specific to SEOCs that may help you:
- SEOC webinar (live and interactive)
- SEOC Quick Reference Guide
- SAR Decision Tool
- SAR Quick Reference Guide
- TriWest Provider Services Phone Staff: 1-866-284-3743, Option 3, Option 4.













